COVID-19 Measures
Personal Protective Equipment (PPE)
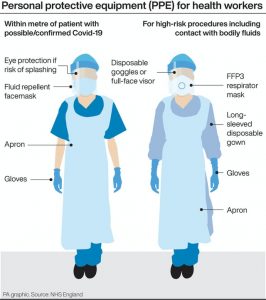 Personal protective equipment (PPE) refers to protective clothing, helmets, gloves, face shields, goggles, facemasks and/or respirators or other equipment designed to protect the wearer from injury or the spread of infection or illness.
Personal protective equipment (PPE) refers to protective clothing, helmets, gloves, face shields, goggles, facemasks and/or respirators or other equipment designed to protect the wearer from injury or the spread of infection or illness.
PPE is commonly used in health care settings such as hospitals, doctor’s offices and clinical labs. When used properly, PPE acts as a barrier between infectious materials such as viral and bacterial contaminants and your skin, mouth, nose, or eyes (mucous membranes). The barrier has the potential to block transmission of contaminants from blood, body fluids, or respiratory secretions. PPE may also protect patients who are at high risk for contracting infections through a surgical procedure or who have a medical condition, such as, an immunodeficiency, from being exposed to substances or potentially infectious material brought in by visitors and healthcare workers. When used properly and with other infection control practices such as hand-washing, using alcohol-based hand sanitizers, and covering coughs and sneezes, it minimizes the spread of infection from one person to another. Effective use of PPE includes properly removing and disposing of contaminated PPE to prevent exposing both the wearer and other people to infection.
When an infection outbreak affects a broad population in the United States, the Centers for Disease Control and Prevention (CDC), is responsible for making specific recommendations for infection control measures in different circumstances and settings. For example, the CDC has provided the following recommendations:
Will personal protective equipment protect against a specific disease?
A2.PPE are designed to create a non-disease specific barrier to penetration of substances, solid, liquid, or airborne particles. In general, neither FDA nor the manufacturer can provide assurances that PPE will protect you against a specific disease. The data that FDA uses for the evaluation and clearance of PPE rarely includes performance evaluation or testing against specific viruses, such as Ebola or flu. If performance data has met FDA requirements and demonstrate protection against a specific disease, the product labeling will state the claim for protection against a specific virus or bacteria.
When there is an outbreak that affects the broad population, The Centers for Disease Control and Prevention (CDC), is responsible for making specific recommendations for infection control measures in different circumstances and settings.
Most dentists and dental practitioners are aware of the need for regular maintenance and disinfection in dental office equipment and tools. However, cleaning the dental chair is an often overlooked – and yet very important – part of routine dental office disinfection procedures.
The dental chair is the one piece of equipment that every single patient who enters the office will use and is designated as a clinical contact surface. Upholstery on the chair is exposed to the spatter of blood, saliva and other body fluids during routine dental care. According to the CDC Guidelines for Infection Control in Dental Health Care Settings, dental patients and staff can be exposed to microorganisms such as:
- Cytomegalovirus
- Permitted disinfectant against bacteria and fungi
- Herpes simplex virus types 1 and 2
- HIV
- Mycobacterium tuberculosis
- Staphylococci
- Streptococci
- Hepatitis B
- Hepatitis C
These organisms can be transmitted through direct contact with blood or body fluids, indirect contact with contaminated objects, inhalational contact with airborne microorganisms and contact with droplets propelled into the air by coughing, sneezing or talking.
In addition, the dental chair is even potentially exposed to parasites such as lice or bed bugs. A poor dental office disinfection and cleaning regimen can potentially expose you, your patients and your staff to these diseases. Dental chair maintenance and disinfection in the dental office are crucial responsibilities for the dentist.
According to the CDC guidelines, impervious barriers can be applied to the surface and would minimize the need for disinfection in dental office equipment. If the barrier were to become compromised or contaminated, then the barrier should be replaced. If these barriers are not used, the surface should be cleaned and disinfected between patients.