Case Studies
GUIDED ERUPTION















A 14 year old female patient reported with a chief complaint of unerupted permanent teeth. Clinical examination revealed the presence of retained deciduous teeth and unerupted permanent teeth. Extraction of retained deciduous teeth was done , Exposure of the impacted permanent teeth was done with LASER and eruption guiding appliance was given. Eruption guidance is a technique where an ideal environment is created for the eruption of the permanent teeth into a perfect Class I relation, with a normal overbite and overjet . The patient was followed up regularly to assess the progress.
IMPLANT







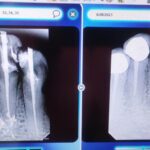
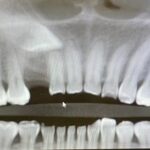
A 49 year old male patient reported to our clinic with a chief complaint of pain in relation to upper front teeth region. On examination it was revealed that the upper front teeth (11) was Root canal treated few years ago. Radiovisiography revealed periapical radioluscency in relation to 11. Also the tooth exhibited grade 3 mobility. The patient was systemically healthy. Extraction and immediate implant was planned and with patient’s consent extraction of 11 was done. A full thickness mucoperiosteal flap was raised. The site was debrided, irrigated and implant of appropriate dimension was placed in relation to 11 site. Bone grafting was done and GTR membrane was adapted to the site. The flaps were approximated and sutured. Post operative instructions were given and the patient was prescribed with analgesics and antibiotics. A Maryland bridge replacing 11 was given provisionally . Also the patient had missing teeth in upper right back teeth region (14 ) and as per his preference a Removable partial denture was given. The patient is kept under follow up .
FULL MOUTH REHABILITATION














Dentistry aims at increasing the longevity of existing dentition. Full mouth rehabilitation encompasses all the procedures necessary to produce healthy teeth with aesthetics, good function and self-maintaining masticatory mechanism. A 54 year old female patient reported with chief complaint of forwardly placed, mobile front teeth and also some decayed teeth. She wanted to replace her existing old fixed bridge prosthesis. On examination the front teeth were periodontally compromised. The patient also had esthetic concerns. With the patient’s informed consent, the anterior teeth were extracted. The existing old fixed bridge was removed. Root canal treatment was carried out in other required teeth and tooth preparations were done. Impressions were made. Facebow bite registration followed by facebow transfer was carried out. Facebow transfers the functional and aesthetic components from patient’s mouth to the dental articulator. After the fabrication of the metal framework , patient was recalled for metal trial and subsequently fixed bridge prosthesis was delivered. The patient was happy to get her smile back.
CYST IN THE ORAL CAVITY

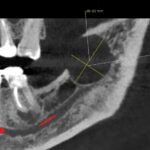







CASE STUDY: A 64 year old female reported with chief complaint of pain in left ear and dizziness since one year. On intra oral examination there was no abnormality found and the patient was referred to ENT specialist and neurologist for an opinion. A CT scan was advised. The CT scan showed a well defined radioluscent cystic mass on the left side in the posterior aspect of mandible. A provisional diagnosis of Residual Cyst was made and a surgical excision of the cyst was planned.
Surgical Procedure: Under local anesthesia, full thickness mucoperiosteal flap was elevated in relation to the left side posterior mandible. The cystic lesion was enucleated, preserving the neurovascular bundle underneath. A big bone defect was observed, and the bone cavity was grafted with sticky bone. Collagen membrane was placed, and the flaps were approximated with resorbable sutures. The excised lesion was sent to lab for histopathological analysis. The patient was prescribed with analgesics and antibiotics and is being followed up.
What are Jaw CYSTS ? Jaw Cysts are relatively rare growths or lesions that could develop in the jawbone or the soft tissues in the mouth and face. Jaw cysts sometimes referred to as odontogenic or nonodontogenic, depending on their origin can vary greatly in size and severity. These growths are usually noncancerous (benign), but they can be aggressive and expand, displace or destroy the surrounding bone, tissue and teeth.
CLEAR ALIGNERS











CASE STUDY: A 37 year old female patient reported with a chief complaint of malposed teeth. On examination it was observed that the patient had Angle’s class 3 malocclusion and anterior open bite. Clear aligners were planned .Maxillary teeth protrusion and mandibular teeth retrusion was done. A significant improvement was noticed . Given below are the images of the patient.
Clear Aligners have become the current trending treatment option for adults preferring to undergo orthodontic tooth correction with esthetic concerns. These aligners are made of clear, BPA-free plastic and are custom-made to fit your teeth. Developments in clear aligner technologies have increased the number and complexity of cases treated with this method . Besides esthetics, Clear aligners provide a comfortable treatment experience, cause less pain as compared to fixed orthodontic appliances, reduce the number and duration of appointments and require less emergency visits. Also Clear aligners facilitate oral hygiene, thus improving the periodontal health and causing a decrease in plaque levels, bad breath, gingival inflammation and bleeding.
Here are some instructions on how to use clear aligners effectively:
Wear as instructed: Clear aligners should be worn for 20 to 22 hours per day, removing them only for eating, drinking (except for plain water), brushing, and flossing. Consistency is key for the treatment to be effective, so make sure to wear your aligners as instructed.
Clean your aligners: It’s essential to keep your aligners clean to maintain good oral hygiene and prevent any odors or staining. Rinse your aligners with lukewarm water every time you remove them, and gently brush them with a soft toothbrush to remove any plaque or debris. Avoid using toothpaste, as it may scratch the aligners.
Brush and floss your teeth: Before reinserting your aligners after meals or snacks, brush your teeth thoroughly and floss. This helps prevent food particles from getting trapped between your teeth and the aligners, reducing the risk of cavities and maintaining good oral health.
Store properly: When not in use, keep your aligners in their designated case to prevent loss or damage. Avoid placing them in tissue or napkins, as they can easily be mistaken for trash and accidentally discarded.
Keep regular check-up appointments: Throughout your treatment, attend all scheduled follow-up appointments with your orthodontist. They will monitor your progress, make adjustments as needed, and provide you with new sets of aligners.
Be patient and consistent: Clear aligner treatment takes time, so it’s important to be patient and follow the instructions diligently. Stick to your treatment plan, wear your aligners consistently, and communicate any concerns or issues you may have with your dentist.
Progress through the aligner sets: Typically, clear aligner treatment involves a series of aligner sets, each designed to gradually move your teeth. Follow the schedule provided by your orthodontist and switch to the next set of aligners as instructed. Each new set will exert gentle pressure on your teeth to continue the alignment process.
Handle aligners with care: Clear aligners are delicate, so handle them with clean hands and avoid bending or twisting them. When removing or inserting the aligners, use gentle pressure and avoid using excessive force, as this may damage them.
ORAL SUBMUCOS FIBROSIS (OSMF)





ORAL SUBMUCOUS FIBROSIS (OSMF)
Oral submucous fibrosis (OSMF) is a chronic, progressive, and potentially debilitating condition that affects the oral cavity. It is characterized by the formation of fibrous bands in the submucosal layers of the mouth, leading to restricted mouth opening, difficulty in chewing, and limited tongue movement. OSMF primarily affects the oral mucosa and the underlying connective tissues, resulting in a variety of symptoms and complications. The exact cause of OSMF is not fully understood, but it is commonly associated with the habitual chewing of areca nut, a common practice in certain regions of Asia. Other factors that may contribute to the development of OSMF include tobacco use, nutritional deficiencies, genetic predisposition, and immune system abnormalities.
Symptoms of OSMF can vary in severity but often include the following:
- Restricted mouth opening: Gradual reduction in the ability to open the mouth fully, leading to difficulty in eating, speaking, and maintaining oral hygiene.
- Thickening and fibrosis of the oral mucosa: The mucosa becomes rigid and leathery, resulting in a loss of elasticity.
- Tongue involvement: The movement of the tongue may be restricted, affecting speech and swallowing.
- Burning sensation and pain in the oral cavity: Patients may experience a burning sensation or pain while eating spicy or hot foods.
- Development of fibrous bands: Fibrous bands may appear as white or pale-colored lines, most commonly observed on the cheeks, palate, and lips.
- Ulcerations and vesicles: In advanced stages, ulcerations or vesicles may be present, leading to discomfort and difficulty in healing.
Diagnosis of OSMF is typically based on clinical examination, medical history, and symptoms reported by the patient. A biopsy may be performed to confirm the diagnosis and rule out other oral conditions.
Treatment of OSMF aims to alleviate symptoms, prevent disease progression, and improve oral function. It often involves a multidisciplinary approach, including the following:
- Cessation of habits: Discontinuation of areca nut chewing and tobacco use is crucial to prevent further damage.
- Medications: Corticosteroids may be prescribed to reduce inflammation and halt the progression of fibrosis. Intralesional injection of dexamethasone 1.5 ml, hyaluronidase 1500 IU with 0.5 ml lignocaine HCL may be administered biweekly. Other medications, such as antioxidants and oral enzymes, may also be used to manage symptoms.
- Laser Biostimulation: Treatment with laser radiation is a safe method of physical therapy that causes regenerative processes in tissues. The treatment is absolutely painless.
4. Physiotherapy: Stretching exercises and mouth-opening devices (Mouth gag) may be recommended to improve mouth opening and maintain oral function.
- Dietary modifications: Patients are advised to avoid spicy, hot, and hard foods that can aggravate symptoms. A well-balanced diet rich in vitamins and minerals is encouraged.
Regular follow-up visits with a dental or oral medicine specialist are necessary to monitor the progression of OSMF and adjust the treatment plan accordingly.
Telescopic Dentures














TELESCOPIC DENTURES
A telescopic denture, also known as a telescoping denture or telescopic prosthesis, is a type of removable dental prosthesis that consists of two parts: an inner coping or primary crown and an outer crown or secondary crown. This design allows for improved retention and stability compared to traditional removable dentures.
The primary coping is fixed onto existing teeth or dental implants in the mouth, while the secondary crown is attached to the removable denture. The secondary crown can be easily inserted and removed from the primary coping, creating a telescopic or sliding mechanism. This design offers several benefits:
1. STABILITY AND RETENTION: The telescopic mechanism enhances the stability of the denture by minimizing movement during speaking and chewing. This reduces the risk of dislodging the denture while eating or speaking.
2. COMFORT: Telescopic dentures often feel more comfortable and secure than traditional removable dentures, as they are less likely to shift or rub against the gums.
3. BETTER CHEWING EFFICIENCY: Improved stability allows for better chewing efficiency, which can positively impact a person’s ability to eat a wider variety of foods.
4. ENHANCED SPEECH: Because the denture is more stable, speech is less likely to be affected by denture movement, resulting in clearer speech.
5. EASE OF MAINTENANCE: Telescopic dentures can be easily removed for cleaning and oral hygiene maintenance.
6. PRESERVATION OF REMAINING TEETH: When used with natural teeth, telescopic dentures can help preserve the remaining tooth structure by distributing chewing forces more evenly.
Telescopic dentures are often recommended for individuals who have a few remaining healthy teeth or dental implants that can serve as support for the primary coping. However, they do require meticulous planning, precise fitting, and regular maintenance. The fabrication of telescopic dentures is a complex procedure that involves careful evaluation of the patient’s oral health, accurate impressions, and collaboration between the dentist and the dental laboratory.
CASE REPORT: A case report of a 61 year old female who reported with chief complaint of loose partial denture in relation to the lower jaw has been described here. Her maxillary complete denture had also worn out. Clinical examination revealed the presence of few lower teeth . Telescopic denture was planned for the lower jaw and a new complete denture for the upper. Root canal treatment was done for the remaining lower teeth . As the teeth had short clinical crown, crown lengthening was carried out and teeth preparations were done. Impressions were made for both upper and lower jaw. Primary copings were fabricated and cemented onto the prepared teeth. Another impression was made and the secondary copings were fabricated and both the upper and lower trial denture was made after bite registration. The final denture was processed after the trial and delivered to the patient. The patient was happy and satisfied with the treatment.
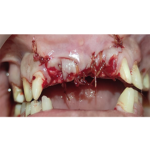
Canine Disimpaction with Immediate Implant Placement







CANINE DISIMPACTION WITH IMMEDIATE IMPLANT PLACEMENT
A 38 year old female patient visited our clinic with complaint of missing front teeth since childhood. Xray and CBCT reports revealed that the upper right permanent canine was impacted under the bone. The patient wanted removal of the impacted teeth. Under local anaesthesia, full thickness flap was elevated and ostectomy was done and the impacted canine was exposed. The tooth was sectioned and extracted and the bone cavity was debrided. Simultaneously an implant of appropriate size was placed in relation to the missing teeth region. Demineralised freeze dried bone allograft with Platelet rich Fibrin (PRF) and collagen membrane were also used to graft the bone defect. The flaps were approximated and closed with resorbable sutures. The patient was prescribed with analgesics and antibiotics and she is being followed up.
